Why Are My Teeth Sensitive? Your Guide to Causes and Relief
That sharp, sudden “zing” you feel when sipping a cold drink is a feeling many of us know all too well. But what's really going on? Why are my teeth sensitive? The short answer is that your tooth's nerve is sending out a pain signal because its protective armor has been weakened, exposing a softer, more porous layer underneath called dentin.
Decoding That Sudden Pain When You Drink Something Cold
If you've ever flinched after a bite of ice cream or a sip of hot tea, you've experienced what's known as dentin hypersensitivity. It’s incredibly common, and understanding the "why" is the first real step toward finding relief that actually lasts.
Think of your tooth like a fortress. The hard, outer enamel is the strong outer wall, built to protect everything inside. Just beneath that wall is the dentin, a layer filled with thousands of microscopic channels, or tubules. These are like tiny tunnels that lead directly to the fortress’s command center—the tooth's nerve, also called the pulp. Under normal circumstances, the enamel and your gums act as gatekeepers, keeping these tunnels sealed off from the outside world.
When the Defenses Are Breached
Sensitivity happens when those defenses are down. If the enamel "wall" thins out from things like acidic foods, or if your gums pull back (recede) like a draining moat, those dentin tubules are suddenly exposed. Now, triggers from the outside have a direct, open pathway to the nerve. This is precisely why certain things cause that familiar jolt of pain.
When dentin is exposed, the nerves within the teeth are far more vulnerable to stimulation. The tiny tubules act as channels, allowing temperature changes and certain food types to rapidly reach the nerve endings, resulting in a sharp, temporary pain.
Knowing what sets off this reaction is a huge piece of the puzzle. To get a better handle on how cold temperatures specifically cause this sensation, you can take a deeper dive in our guide on the causes of tooth sensitivity to cold.
Common Triggers for Tooth Sensitivity
Certain foods, drinks, and even the air we breathe can be notorious for setting off a sensitive response. Here’s a quick-reference table of the most frequent offenders and why they cause that distinct pain.
| Trigger | Why It Causes Pain |
|---|---|
| Cold Foods & Drinks | A rapid drop in temperature causes the fluid inside the dentin tubules to move quickly, stimulating the nerve. |
| Hot Foods & Drinks | Similar to cold, extreme heat also causes that same fluid movement within the tubules, triggering a pain signal. |
| Sweet or Sugary Foods | Sugar changes the fluid balance around the tubules through osmosis, which irritates the nerve endings. |
| Acidic Foods & Drinks | Acids from citrus fruits, soda, or wine can further wear down enamel and directly irritate the exposed dentin. |
While recognizing these triggers is helpful for avoiding immediate pain, the real key to long-term relief is figuring out why your tooth’s defenses were compromised in the first place and addressing that root cause.
Uncovering the Root Causes of Your Tooth Sensitivity
That sharp, sudden zing of pain is more than just a minor annoyance—it's your teeth sending out an S.O.S. To find a real, lasting solution, we have to play detective and figure out what’s actually causing the problem. The question "why are my teeth sensitive?" rarely has just one answer, and zeroing in on the specific culprit is your first step toward relief.
Think of it like this: a compromised enamel shield leads to exposed dentin, which creates a direct, open line to the nerve.
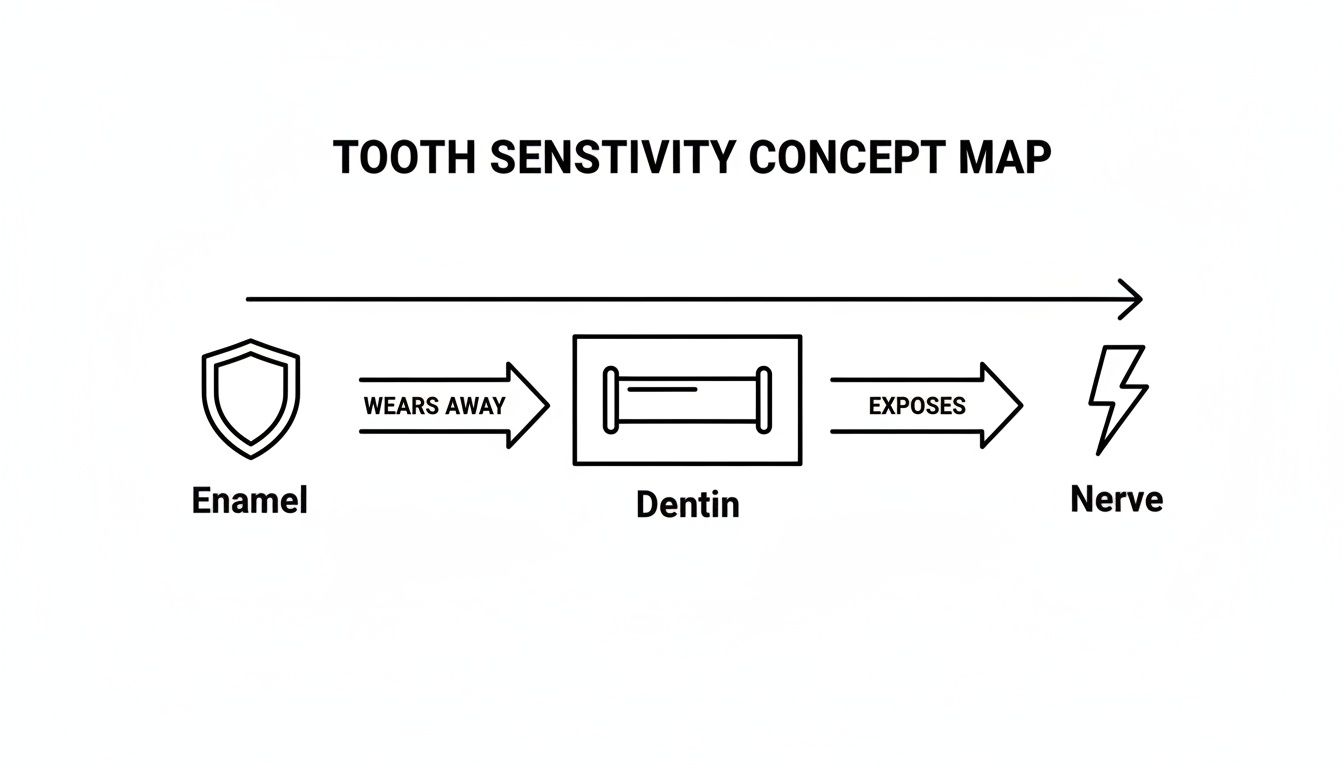
This visual journey from the outer armor to the inner nerve shows how the breakdown of your tooth's defenses is the central event in developing sensitivity. Let's break down the most common ways this happens.
Worn-Down Enamel: Your Tooth's Eroding Shield
Imagine your tooth enamel as a tough, durable shield. Over time, that shield can wear down in a process known as enamel erosion. The main offender here is frequent exposure to acids from everyday foods and drinks—think citrus fruits, sodas, and even your morning coffee.
When acid hits the enamel, it’s like a slow, steady weathering of a stone monument. You won't see the changes at first, but over years, the enamel thins out, revealing the softer, more porous dentin layer underneath. This erosion basically punches tiny holes in your tooth's armor, creating a pathway for hot, cold, and sweet sensations to jolt the nerve.
Receding Gums: Exposing Vulnerable Roots
Your gums are just as critical in protecting your teeth. They create a tight seal around the base of each tooth, covering the root surfaces, which don't have that hard enamel coating.
When gums pull back, or recede, they leave this sensitive root area exposed. It’s a lot like a receding shoreline revealing the vulnerable land beneath it. Gum recession is a huge contributor to sensitivity and can be triggered by a few different things:
- Aggressive Brushing: Using a hard-bristled brush or just scrubbing way too hard can physically wear away your gum tissue.
- Gum Disease: Inflammation from gingivitis or more advanced periodontal disease can cause the gums to detach and pull away from the teeth.
- Age: It's natural for gums to recede a bit as we get older.
In fact, clinical research has found that gingival recession—receding gums—is the single biggest cause of tooth sensitivity. It's responsible for roughly 66% of all sensitivity cases simply by exposing the dentin on the tooth's root.
The Impact of Physical Force and Habits
Beyond acids and gum issues, direct physical stress on your teeth is another major cause of sensitivity. This often happens without you even noticing. Two of the biggest culprits are teeth grinding and overly aggressive brushing habits.
Teeth grinding, clinically known as bruxism, puts a massive amount of pressure on your teeth, usually while you're asleep. This constant force can wear down enamel and even cause tiny fractures. In the same way, abrasion from harsh brushing can literally scrape away both enamel and the cementum (the thin layer covering the root), creating painful, sensitive spots.
Digging into the clinical data reveals just how common these factors are. According to extensive research, 66% of sensitivity cases are tied to gum recession, while mechanical wear from abrasion and erosion is a factor in 59% of cases. On top of that, bruxism contributes to 32% of sensitivity instances, as the grinding action speeds up both enamel wear and gum recession. These numbers really show how much our daily habits can impact tooth health. To see the full breakdown, you can explore the research on sensitive teeth management.
Other Common Causes of Sensitivity
While the issues above are the most frequent offenders, a few other things can bring on that familiar painful zing. It's worth keeping these in mind as you try to pinpoint the source of your discomfort.
- Cracked or Chipped Teeth: Even a tiny, hairline crack can create a direct highway to the dentin or nerve, causing sharp, localized pain.
- Tooth Decay (Cavities): As a cavity forms, it eats through the enamel, exposing the sensitive dentin layer and causing sensitivity that often gets worse over time.
- Recent Dental Work: It’s totally normal to feel some temporary sensitivity after procedures like professional cleanings, fillings, crown placements, or teeth whitening. The process can irritate the nerve for a bit, but this feeling usually fades within a few days or weeks.
Figuring out which of these root causes applies to you is the key. Once you've identified the "why" behind your sensitivity, you can start choosing the right treatments and prevention strategies to protect your smile for good.
How Dentists Pinpoint the Cause of Sensitivity
If you're dealing with sensitive teeth, the single most important thing you can do is see your dentist. It’s not just about getting confirmation that something hurts; it’s about figuring out the why. A professional diagnosis is the only way to get on the right track and find a treatment that actually works.
Think of your dentist as a detective. They're looking for clues inside your mouth, using a mix of visual checks, specific tools, and the right questions to rule out other problems that can feel a lot like sensitivity, such as a hidden cavity or even an abscess.
The Diagnostic Examination
Your visit will start with a conversation. Your dentist needs to understand exactly what you're feeling, so they'll ask when the pain started, which teeth are giving you trouble, and what sets it off. Is it a sharp zing or more of a dull ache? Does the pain vanish instantly or does it linger? These details are the first clues to narrowing down the list of suspects.
Next comes a careful visual inspection. They're searching for the tell-tale signs that point to the usual culprits behind sensitivity.
- Evidence of Wear: Your dentist will look for thinned-out enamel or flattened chewing surfaces. This can be a dead giveaway for erosion caused by acidic foods or the immense pressure from grinding your teeth at night (bruxism).
- Gum Recession: They’ll check your gum line to see if the tissue has pulled back anywhere. When this happens, it exposes the tooth's sensitive root surfaces, which aren't meant to be out in the open.
- Cracks or Damage: With specialized lights and magnification, a dentist can spot tiny, hairline fractures that you'd never see on your own. Even a small crack can create a direct pathway to the nerve, causing a jolt of pain.
This initial once-over gives your dentist a solid idea of what might be going on.
Specialized Tests for Pinpointing Pain
After the visual check, your dentist might use a few gentle tests to zero in on the problem tooth and confirm their suspicions. These methods are designed to safely replicate your symptoms in a controlled way, so they can get an accurate picture of the problem.
One of the most common is the "air test." Your dentist will use a small instrument to direct a gentle puff of air onto a specific tooth. If exposed dentin is the issue, this sudden change in temperature will trigger that familiar sharp sensation, confirming exactly where the discomfort is coming from.
A proper diagnosis is the foundation for effective treatment. Without identifying the root cause—be it enamel erosion, gum recession, or a cracked tooth—any at-home remedies or treatments are simply shots in the dark.
They might also try gently tapping on individual teeth (percussion) or having you bite down on a small stick. These simple tests help them figure out if the pain is originating from the tooth's nerve or from the surrounding ligaments, which is crucial for distinguishing sensitivity from a cracked tooth or an infection. Sometimes, X-rays are also needed to spot decay hiding between teeth or to check on existing fillings and the underlying bone.
Understanding this process makes it clear why guessing at the cause of your sensitivity just doesn't cut it. When you work with a dentist, you get a clear diagnosis that leads to a targeted, effective treatment plan—and that's how you finally find real, lasting relief.
Finding At-Home Relief That Actually Works
When that sharp jolt of pain from sensitive teeth interrupts your day, you want a solution that works—and fast. The good news is you don't always have to wait for a dental appointment to start tackling the problem. Your local pharmacy aisles are full of effective, evidence-based products designed specifically to bring you relief.
Understanding how they work is the key to picking the right tool for the job.

If you're dealing with sensitivity, you're far from alone. A massive European study of over 3,500 adults found that more than 50% of participants experienced some form of dentin hypersensitivity. But despite how common it is, about half of them weren't actively doing anything to treat it. This shows a huge gap between feeling the pain and finding relief. You can read the full study to learn more about these findings.
Desensitizing Toothpastes: Your First Line of Defense
The easiest place to start is with a desensitizing toothpaste. While they all aim to reduce pain, they go about it in a couple of different ways, using specific active ingredients to get to the source of the problem.
Think of them as having two main strategies: calming the nerve or blocking the pain pathways.
One of the most common ingredients you'll see is potassium nitrate. This compound works like a peacekeeper for your tooth's overactive nerve. With regular brushing, it gradually builds up around the nerve, making it less excitable and less likely to fire off pain signals when you have that cold drink or sweet snack.
Another powerhouse ingredient is stannous fluoride. This multi-tasker takes a different approach. It acts like a spackle, creating a thin, protective barrier over the exposed parts of your tooth. More importantly, it helps plug the microscopic dentin tubules—those tiny tunnels leading to the nerve. By blocking these pathways, stannous fluoride cuts off the route that triggers use to reach the nerve in the first place.
Rebuilding Your Enamel with Fluoride Rinses
Beyond a good toothpaste, adding a fluoride rinse to your routine gives you another critical layer of support. Fluoride is a mineral that essentially acts as a repair crew for your enamel, which is your tooth's natural protective shield.
Every time you eat or drink something acidic, your enamel loses minerals in a process called demineralization. This weakens it, making it thinner and more prone to wear, which is a fast track to sensitivity. Fluoride helps reverse this damage through remineralization. It gets absorbed into the enamel, replenishing those lost minerals and making your teeth stronger and more resistant to future acid attacks.
By using a combination of products that calm the nerve, block the dentin tubules, and strengthen your enamel, you are creating a comprehensive, multi-layered defense system against tooth sensitivity.
This triple-action approach is a fantastic way to manage generalized sensitivity from home.
Targeted Treatments for Stubborn Spots
Sometimes, the sensitivity isn't all over, but concentrated in one or two particularly annoying spots. For those cases, more targeted treatments like desensitizing gels can be a game-changer. These gels often contain higher concentrations of active ingredients like potassium nitrate or fluoride.
You apply them directly to the sensitive areas, letting the ingredients get to work right where you need them most. This direct application can provide more potent and faster relief for that localized "zing." If this sounds like what you're dealing with, our guide on desensitizing gel for teeth dives deeper into how these products can help.
With so many options, picking the right one can feel overwhelming. This table breaks down the most common products to help you find the best fit.
Choosing Your At-Home Sensitivity Treatment
| Product Type | How It Works (Analogy) | Best For | Example Product (Brand) |
|---|---|---|---|
| Potassium Nitrate Toothpaste | Nerve Calmer: It's like putting noise-canceling headphones on an overactive nerve. | Daily management of generalized, mild-to-moderate sensitivity. | Sensodyne |
| Stannous Fluoride Toothpaste | Tubule Blocker: It's like a construction crew patching up tiny potholes on a road. | Sensitivity caused by enamel erosion and exposed dentin. | Crest Pro-Health |
| Fluoride Rinse/Mouthwash | Enamel Rebuilder: It's like a vitamin supplement that strengthens your tooth's outer shell. | Preventing future sensitivity and strengthening weak enamel. | ACT Restoring |
| Desensitizing Gel | Spot Treatment: It's like applying a concentrated pain-relief cream directly to a sore muscle. | Intense, localized sensitivity on one or two specific teeth. | MI Paste ONE |
No matter which product you start with, consistency is key. These treatments work by building up protection over time, so stick with your new routine to give it a chance to work. By understanding the science behind each option, you can confidently choose the right defense for your smile.
When Your Tooth Sensitivity Needs a Dentist's Help
While sensitivity toothpastes and fluoride rinses are fantastic first lines of defense, some situations are simply beyond the scope of at-home care. The real trick is knowing how to tell the difference between minor, manageable sensitivity and a red flag that needs a professional eye. If you ignore certain symptoms, a small issue can snowball into a much bigger problem.
Think of it this way: a fleeting twinge from a cold drink is like a brief weather alert you can mostly ignore. But sharp, lingering pain? That’s a persistent storm warning telling you to take cover—and in this case, that means seeing your dentist.
Key Warning Signs to Watch For
If you’re dealing with any of the following, it’s a clear sign to put down the over-the-counter products and book a dental appointment. These symptoms often point to an underlying problem that no amount of special toothpaste can fix on its own.
- Pain That Lingers: If the sensitivity hangs around for more than a minute after you've finished your hot coffee or cold water, it might mean there's a deeper issue with the tooth's nerve.
- Sharp Pain When Biting: A specific, sharp pain right when you bite down is a classic sign of a cracked tooth, a loose filling, or decay that’s reached a critical point.
- Sensitivity in a Single Tooth: While general sensitivity is pretty common, intense pain that’s zeroed in on one particular tooth often signals a focused problem, like a cavity or even an abscess.
- No Improvement After Weeks: You've been diligent with desensitizing products for several weeks but are getting zero relief. It's time for a dentist to figure out what's really going on.
- Visible Tooth Damage: If you can see a new chip, crack, or a dark spot on the tooth that's bothering you, that’s your cue to get it checked out professionally.
- Swollen or Bleeding Gums: When sensitivity comes with red, puffy, or bleeding gums, it could be a sign of advancing gum disease, which definitely requires professional treatment.
While tooth sensitivity is incredibly common, it often goes underdiagnosed. It’s one of the top complaints we hear in the dental chair, yet so many people wait it out, just hoping the problem will disappear on its own.
This is a familiar story. Research shows that while 25-30% of adults struggle with tooth sensitivity, it remains one of the most underdiagnosed dental conditions out there. You can explore the research on sensitivity prevalence to see just how widespread it is. This gap between experience and diagnosis is exactly why being your own health advocate is so important.
At the end of the day, you know your body best. If the pain feels severe, keeps getting worse, or just doesn't feel "right," trust that instinct. A quick visit to the dentist will get you a proper diagnosis and the right treatment to not only stop the pain but fix the root cause for good.
Your Action Plan for Preventing Future Sensitivity

Knowing why your teeth are sensitive is half the battle, but taking back control means getting proactive. The best way to deal with sensitivity is to stop it before it starts—or at least keep it from getting worse. This straightforward plan is all about building simple, daily habits that will protect your teeth for the long haul.
Think of your tooth enamel as your smile’s first line of defense. Keeping it strong and intact is the single most important part of preventing sensitivity. It all starts with something as simple as how you brush. Scrubbing away aggressively with a hard-bristled brush can wear down both your enamel and your delicate gums, which can lead to recession and exposed dentin.
Instead, make a conscious effort to switch to a soft-bristled toothbrush and use gentle, circular motions. The idea is to clean your teeth, not scour them like a dirty pan. That small change alone can make a huge difference in reducing the kind of physical wear and tear that leads to sensitive teeth.
Fortify Your Defenses Daily
What you eat and how you clean your teeth play a massive role in keeping your enamel tough. Acids from the foods and drinks we enjoy every day are one of the biggest culprits behind enamel erosion, so being a little more mindful can go a long way.
Here are a few essential habits to build into your daily routine:
- Limit Acidic Foods and Drinks: Things like soda, citrus fruits, and wine can temporarily soften your enamel. When you do have them, just swish your mouth with some water afterward to help neutralize the acid.
- Wait Before You Brush: Right after you have something acidic, your enamel is in a weakened state. Give it at least 30 minutes to reharden before you brush to avoid scrubbing away that vulnerable layer.
- Use Fluoride Consistently: Fluoride is a mineral that actively helps rebuild and strengthen your enamel. Make sure your daily toothpaste or mouth rinse has it on the ingredient list.
Prevention really just comes down to creating a healthy environment in your mouth where your enamel can thrive. Small, consistent actions add up to build a powerful defense against the things that trigger tooth sensitivity.
If you want to take it a step further, there are plenty of other proven ways to strengthen tooth enamel that can give you an extra layer of protection.
Address Underlying Habits
Finally, it’s crucial to tackle any habits that are putting too much force on your teeth. A common offender is teeth grinding (also called bruxism), which can wear down your enamel much faster than normal.
If you think you might be grinding your teeth at night—tell-tale signs include a sore jaw or headaches when you wake up—it’s time to chat with your dentist. They can get you fitted for a custom nightguard. This simple device acts as a cushion between your top and bottom teeth, absorbing the pressure and shielding your enamel from all that grinding. By combining these gentle habits, you can build a robust defense and keep sensitivity from taking over your life.
Common Questions About Tooth Sensitivity
When you're dealing with that sharp zing of tooth sensitivity, you're bound to have questions. It's one of the most common complaints we hear about. Let's clear up some of the confusion and tackle the questions people ask most often.
Can Teeth Whitening Cause Permanent Sensitivity?
This is a big one, and thankfully, the answer is pretty straightforward: no, professional teeth whitening won't cause permanent sensitivity. Here’s what’s happening: the peroxide agents used in whitening gels temporarily open up the pores in your enamel. This is how the gel gets in to lift stains from the underlying dentin layer.
This increased porosity is what triggers that temporary sensitivity to hot and cold foods. But it's a short-lived effect. Within a few days after your treatment, your enamel naturally remineralizes and rehydrates, and that sensitivity fades away. It’s a world away from the chronic sensitivity caused by things like enamel erosion or receding gums, which are ongoing structural problems.
Does Tooth Sensitivity Ever Go Away on Its Own?
It's tempting to take a "wait and see" approach, but in most cases, tooth sensitivity won't just vanish on its own. That's because sensitivity is almost always a symptom of a physical change to your tooth structure, like worn-down enamel or exposed tooth roots from gum recession.
Unfortunately, these conditions don't reverse themselves. Once enamel is gone, it's gone for good. And gums that have receded won't magically grow back to their original position.
You can think of ignoring tooth sensitivity like ignoring a leaky roof. It’s a structural issue, and it will stick around—and probably get worse—until you take active steps to fix the problem or manage the cause.
This is why active management is key. That usually means using desensitizing products to calm the nerve signals or, better yet, working with your dentist to get to the root of the problem, whether that requires a filling, a nightguard for grinding, or treatment for gum issues.
Are Natural Remedies Like Oil Pulling Effective?
While oil pulling—the practice of swishing oil in your mouth—has gained popularity for general oral wellness, there's no solid scientific evidence showing it's an effective treatment for dentin hypersensitivity. The idea is that it can reduce bacteria, but it doesn’t actually address the mechanical problems causing the sensitivity, like open dentin tubules or worn enamel.
Clinically proven treatments work in very specific ways. Ingredients like potassium nitrate work by calming the tooth's nerve, while others like stannous fluoride work by physically plugging the microscopic tubules in your dentin. These ingredients have gone through rigorous testing to prove they work. While something like oil pulling is generally harmless, you'll get much more reliable relief by sticking to evidence-based treatments.
Why Did My Teeth Become Sensitive All of a Sudden?
When sensitivity pops up out of nowhere, it can be pretty alarming. Unlike the gradual sensitivity that builds over years from wear and tear, sudden pain is often your mouth's way of sending up a flare gun—it's signaling a new, specific problem that needs immediate attention.
Some of the most common culprits include:
- A New Cavity: Tooth decay can chew through enamel surprisingly quickly, exposing the sensitive dentin layer underneath.
- A Cracked or Chipped Tooth: Even a microscopic fracture can create a direct line to the nerve, causing a sharp, immediate jolt of pain.
- Recent Dental Work: It's completely normal to have some temporary sensitivity after a filling, crown, or even a professional cleaning while the tooth and surrounding gums settle down.
If you experience a sudden onset of sensitivity, that's a clear sign to call your dentist. They can pinpoint the exact cause and get you the right treatment to stop the pain and fix the underlying issue.

