How to Relieve Tooth Sensitivity After Whitening
That sharp little zing you feel after a whitening treatment can be alarming, but it’s actually incredibly common and, thankfully, temporary. The whitening agents are designed to open up microscopic pores in your tooth enamel to lift out stains. In doing so, they briefly expose the more sensitive layer underneath, which is what's causing that discomfort.
Understanding Why Whitening Causes Tooth Sensitivity

If you've just wrapped up a whitening session and now the mere thought of a cold drink makes you wince, you're in good company. This is a normal part of the process for a lot of people. It’s not a red flag for damage; it’s just a temporary side effect of the whitening gel doing its job effectively.
The active ingredients in most whitening gels, like hydrogen peroxide or carbamide peroxide, are fantastic at breaking down stubborn stains. To get to those stains, they need to pass through the enamel, your tooth's protective outer layer. This process temporarily makes the enamel more porous, opening up tiny channels that lead straight to the tooth's nerve center, known as the dentin.
The Science Behind the Sensation
Once those microscopic pathways are open, external triggers can send a jolt straight to the nerve. It’s a bit like opening a window on a chilly day—you suddenly feel the cold air that was blocked before. For your teeth, common triggers include:
- Temperature: Hot coffee and ice-cold water are the usual suspects.
- Sweetness: Sugary foods and drinks can also cause a sharp sensation.
- Acidity: Things like citrus fruits, sodas, and even some tangy salad dressings can be provocative.
- Air: Sometimes, even breathing in crisp, cold air is enough to make you uncomfortable.
The intensity of this sensitivity often depends on the strength of the whitening agent. A high-concentration professional treatment might cause more noticeable sensitivity than a gentler at-home kit.
The key takeaway is that post-whitening sensitivity is a physiological response, not an indication of permanent harm. Your enamel will naturally remineralize and rehydrate, and the discomfort will fade.
How Common Is Whitening Sensitivity?
This is a really common experience. Studies show that more than 50 percent of patients feel some level of sensitivity after a whitening treatment.
One in-depth clinical study looked at people using at-home kits with 16% carbamide peroxide. They found about 54% reported mild sensitivity, 10% had moderate sensitivity, and just 4% experienced severe sensitivity. The good news is that for most people, this discomfort is short-lived, usually resolving on its own within one to two weeks.
Just knowing this is a normal part of the process is the first step. It helps shift your focus from worrying about damage to finding smart ways to manage it, which is exactly what we're about to get into. If you're curious about the broader causes of tooth pain, you might want to check out our guide on why teeth become sensitive.
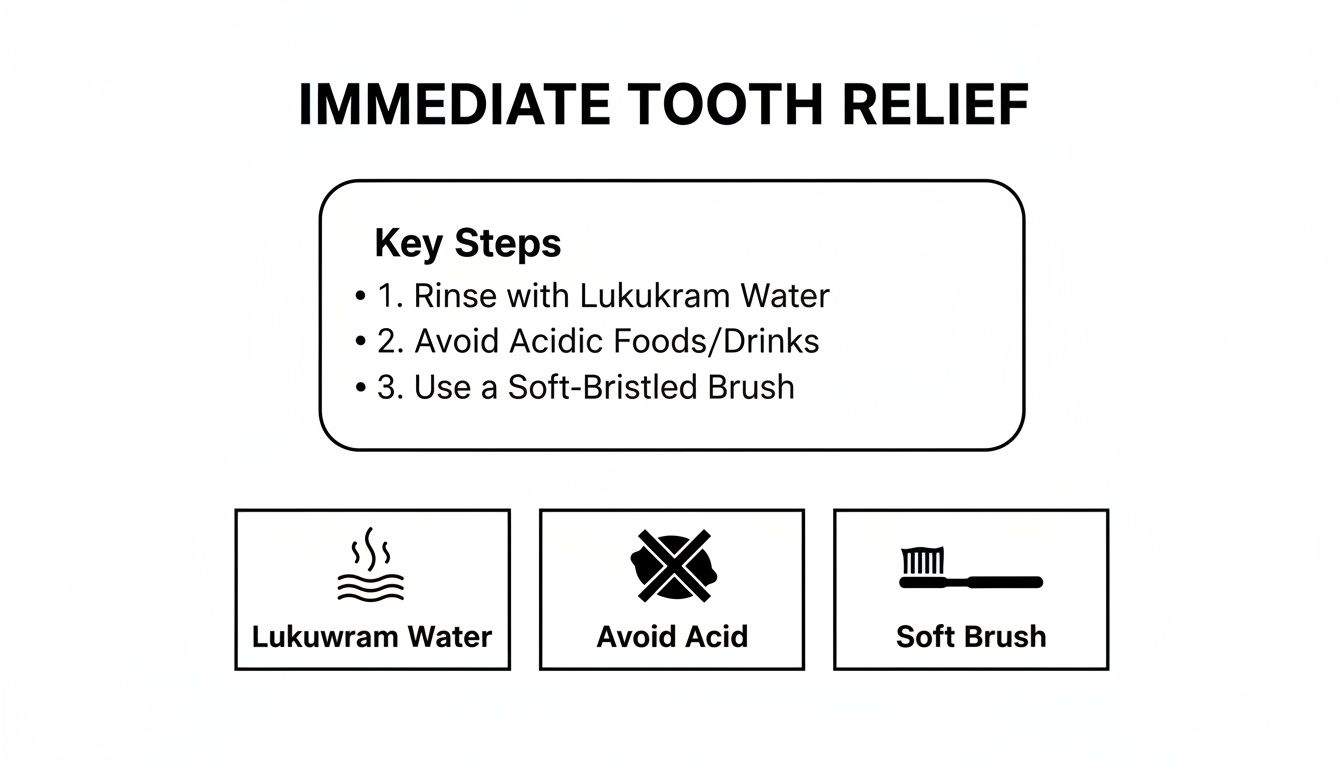
Finding Immediate Relief for Sensitive Teeth
When that sharp zing of sensitivity hits after a whitening treatment, you want relief now, not in a few days. That discomfort is just a signal that your tooth's nerve endings are temporarily a bit exposed and need some TLC. The good news is, you can take simple, immediate steps at home to calm them down and feel better fast.
Your first line of defense is often the easiest: manage the temperature of what you eat and drink. For the first 24 to 48 hours, just swapping out ice water for room-temperature water can make a massive difference. Same goes for your morning coffee or tea—let it cool down a bit before you take a sip. You want to avoid shocking those sensitive nerves.
Simple At-Home Soothing Rinses
A gentle, lukewarm salt water rinse is a classic remedy for a reason. Salt is a natural anti-inflammatory, which can help soothe irritated gum tissue and dial down that overall oral discomfort.
Just mix half a teaspoon of salt into an eight-ounce glass of warm water. Swish it around your mouth for about 30 seconds, then spit it out. You can do this two to three times a day to help everything calm down.
Remember, the goal here is immediate comfort. These small adjustments aren't just suggestions; they are practical ways to actively reduce the triggers causing your sensitivity, giving your teeth the peaceful break they need to recover.
Another key strategy is just being mindful of what you eat. Your teeth are extra vulnerable right after whitening, and acidic foods can feel like pouring lemon juice on a paper cut.
For a day or two, try to sidestep things that can aggravate sensitivity:
- Citrus Fruits like oranges, lemons, and grapefruits.
- Tomatoes and any tomato-based sauces.
- Carbonated Drinks, including both soda and sparkling water.
- Wine, which is not only acidic but can also cause staining.
The Importance of a Gentle Touch
How you brush your teeth right now matters immensely. If you're an aggressive brusher, you can make sensitivity much worse by irritating your teeth and gums even more.
Switch to a soft-bristled toothbrush and use a light, gentle touch. Think of it as polishing, not scrubbing. This simple change stops you from adding unnecessary physical pressure to the temporary sensitivity.
For more targeted relief, some people find great success with products specifically designed to calm those nerves. If you want to learn more, you can explore our guide on how teeth desensitizing gels work.
The best part is that this discomfort is almost always short-lived. Research shows that sensitivity typically lasts up to 48 hours after whitening for most people, though it can vary. While some feel better within a day, others might notice it for up to a week. The most reassuring part? No studies have ever shown this sensitivity to cause any irreversible damage. You can find more insights about these temporary whitening effects at healthcare.utah.edu.
Building Your Post-Whitening Care Kit
Those immediate fixes feel great, but a smart oral care routine is your best bet for lasting comfort and preventing future sensitivity. This isn't about running out and buying a bunch of random products; it's about putting together a targeted kit to soothe, strengthen, and protect your newly whitened smile.
The right products work together to calm down overactive nerves and rebuild your tooth enamel. By folding just a few key items into your daily habits, you can stop dreading that cold glass of water and really enjoy your brighter smile.
These initial steps are crucial. They create a baseline of comfort so your specialized products can do their job without having to fight against constant irritation.
Start with a Desensitizing Toothpaste
The MVP of your anti-sensitivity routine is a quality desensitizing toothpaste. These are specially formulated with active ingredients clinically proven to tackle sensitivity head-on. You'll want to look for formulas that contain either potassium nitrate or stannous fluoride.
- Potassium Nitrate: Think of this as a nerve-calming agent. It works its way into the tooth to soothe the nerve, intercepting pain signals before they can even register. The relief builds up over time with consistent use.
- Stannous Fluoride: This one is all about building a defensive shield. It creates a barrier over the tiny, microscopic tubes in your dentin, physically blocking triggers like cold air or sweet foods from ever reaching the nerve.
Here’s a little trick I recommend to my patients: before you start brushing, dab a small amount of the sensitivity toothpaste directly onto the most sensitive teeth. Let it sit for a minute or two. This direct contact gives the active ingredients a head start right where you need it most.
Strengthen and Rebuild with Fluoride & Remineralizing Pastes
Beyond just blocking pain, the real long-term goal is to reinforce your enamel. The whitening process can temporarily make your enamel more porous, and strengthening it back up is key. This is where fluoride and special remineralizing pastes come into play.
Adding a daily fluoride rinse to your routine after brushing is an easy and effective way to help remineralize your enamel, making it stronger and less permeable.
For a more intensive treatment, look into products like MI Paste. These are remineralizing pastes packed with bio-available calcium and phosphate—the very building blocks of your tooth structure.
Using a remineralizing paste is like giving your teeth a deep conditioning treatment. It actively replenishes lost minerals, helping to seal up those porous channels and build a much more robust shield against sensitivity triggers.
To help you choose the right tools for your kit, here’s a quick breakdown of how these products differ and when to use them.
Comparing Sensitivity Relief Products
| Product Type | Primary Function | Key Active Ingredients | Best For |
|---|---|---|---|
| Desensitizing Toothpaste | Blocks pain signals & creates a protective barrier | Potassium Nitrate, Stannous Fluoride | Daily, ongoing management of mild to moderate sensitivity. |
| Fluoride Rinse | Strengthens and hardens enamel | Sodium Fluoride | Daily use after brushing to fortify teeth against future sensitivity. |
| Remineralizing Paste | Rebuilds enamel by replenishing lost minerals | Calcium, Phosphate (e.g., RECALDENT™ in MI Paste) | Intensive repair for moderate to severe sensitivity or after whitening. |
Ultimately, combining these products creates a powerful, multi-pronged defense. The toothpaste provides immediate and ongoing relief, while the fluoride rinses and remineralizing pastes get to work rebuilding and fortifying your teeth for the long haul. This combo strategy is one of the most effective ways to knock out post-whitening sensitivity for good.
Whitening Smarter to Prevent Future Pain

While all these tips for managing sensitivity work wonders, the best strategy is to avoid the pain in the first place. You can absolutely achieve that brilliant smile without the uncomfortable side effects by taking a proactive approach to your next whitening session. It’s all about creating a smart, personalized plan that prioritizes both results and comfort.
The single biggest factor behind post-whitening sensitivity is the strength of the bleaching agent. It’s tempting to grab the highest concentration you can find, thinking it will work faster. But this is often a fast track to serious discomfort. A much more strategic approach is to simply choose a product with a lower peroxide concentration.
Choose a Gentler Whitening Gel
Lower-strength gels can deliver beautiful, bright results over a slightly longer period—but with a much lower risk of pain.
For example, a gel with 10% carbamide peroxide is what we often recommend for anyone with a history of sensitivity. It works more gradually than its high-strength counterparts, which gives your teeth plenty of time to adapt to the process.
Research backs this up. One clinical study comparing different whitening methods found that a powerful 40% hydrogen peroxide in-office treatment caused the most significant spike in sensitivity. Meanwhile, an at-home treatment using 10% carbamide peroxide resulted in the lowest increase in sensitivity scores. This makes it a clear winner for anyone prone to zings.
Adjust Your Whitening Schedule and Timing
Your whitening routine shouldn't be rigid. One of the most powerful tools you have is simply listening to your body and adjusting your schedule as needed. More whitening isn't always better, especially if it causes pain that forces you to quit altogether.
Consider making these easy adjustments to your routine:
- Shorten Your Sessions: If the box says to wear the trays for 60 minutes, try 30 minutes instead. You’ll still get whitening benefits with less exposure for your enamel.
- Skip a Day (or Two): Whitening every single day can be too intense for some teeth. Switching to an every-other-day schedule gives your teeth a crucial recovery period to rehydrate and remineralize between sessions.
- Whiten Before Bed: Applying the treatment at night can be a game-changer. Saliva production naturally decreases while you sleep, allowing the gel to work with less interruption. Plus, you’ll sleep right through the initial period when sensitivity might be at its peak.
The real goal is consistency over intensity. A comfortable, sustainable routine will always deliver better long-term results than an aggressive approach you can't maintain.
Use Desensitizing Products Before You Whiten
This is one of my favorite pro tips. One of the most effective preventative strategies is to prepare your teeth before the whitening agent ever touches them. By using desensitizing products in advance, you can build up your teeth's defenses and block pain pathways before they even get activated.
Start by switching to a desensitizing toothpaste containing potassium nitrate or stannous fluoride about two weeks before you plan to whiten.
For an even bigger impact, apply a desensitizing gel directly to your teeth in your whitening trays for 10-20 minutes right before your actual whitening session. This preemptive strike helps block the microscopic tubules in your dentin, creating a shield that prevents the whitening gel from triggering nerve pain.
Our guide on hydrogen peroxide gels can help you learn more about how different product formulations work and what to look for.
Knowing When to Call Your Dentist
Most of the time, that zingy feeling you get after whitening is a totally normal, temporary side effect. But it's really important to know the difference between a typical reaction and a genuine red flag.
Think of it as a safety check. A little sensitivity for a day or two is one thing; persistent, sharp pain is another story entirely and definitely warrants a call to your dentist.
Your discomfort should get better each day, and it usually disappears completely within a week after you finish your last whitening treatment. If the pain isn’t fading—or it’s actually getting worse—it’s time to pick up the phone. Don't try to "tough it out," especially if it’s interfering with your ability to eat, drink, or just get through your day.
Identifying Concerning Symptoms
Knowing exactly what to look for can help you decide if it's time to make that call. While a mild, all-over sensitivity is pretty much expected, some symptoms are absolutely not part of the normal whitening process.
Be on the lookout for these warning signs:
- Severe, Unmanageable Pain: This is pain that just laughs at over-the-counter remedies and sensitivity toothpastes. If nothing is touching the discomfort, that's a problem.
- Pain Lasting More Than a Week: If you've finished whitening and the sensitivity is still hanging around a week later, something else might be going on.
- Localized, Sharp Pain: A constant ache or a sharp "zing" in one specific tooth is different from generalized sensitivity and needs to be checked out.
- Swollen or Bleeding Gums: Whitening gels can definitely irritate your gums, but significant swelling, blistering, or bleeding is not normal.
- White Patches on Gums: This can be a sign of a chemical burn from the peroxide gel, which a dentist needs to look at.
Why These Symptoms Matter
These symptoms are often more than just side effects; they can be signals of an underlying issue that the whitening process has stirred up.
For instance, a sharp pain in one specific spot could point to an undiagnosed cavity or a tiny crack in a tooth. When the whitening gel seeps into these compromised areas, it can cause a level of pain far beyond typical sensitivity.
Likewise, serious gum irritation might mean you have pre-existing gum recession. When the root of the tooth is exposed, it doesn't have that protective layer of enamel, making it extremely vulnerable to the peroxide in whitening agents.
Calling your dentist isn't an overreaction; it's a smart, proactive step. A quick check-up can rule out serious problems, get you prescription-strength relief if needed, and make sure your oral health is solid before you try to whiten again. It's all about peace of mind and protecting your smile for the long haul.
Your Questions on Whitening Sensitivity Answered
When you're trying to get a brighter smile, a few questions always pop up, especially about that super common sensitivity issue. Getting some clear, honest answers can make the whole process feel way less intimidating. Let's dig into the most frequent questions people have about balancing a whiter smile with real comfort.
Knowing the ropes helps you whiten smarter, not harder. You can get amazing results without having to just put up with days of zings and aches.
Can I Whiten My Teeth If They Are Already Sensitive?
Absolutely, but you have to be smart about it. The secret is to prep your teeth beforehand to help them build up some resilience against sensitivity. A great first step is switching to a desensitizing toothpaste at least two weeks before you plan on starting your whitening treatment.
This gives the active ingredients, like potassium nitrate, enough lead time to really get in there and calm down the nerves inside your teeth. For an even more comfortable experience, think about making these adjustments:
- Go for a lower peroxide concentration: Choose a gentler whitening formula. It might take a little longer to see the final results, but you'll get there with way less irritation.
- Space out your sessions: Instead of whitening every single day, try doing it every other day. This gives your teeth a crucial 24-hour break to recover and rehydrate between treatments.
- Add a remineralizing paste: Using a product like MI Paste after you whiten helps put essential minerals back into your enamel, making it stronger.
How Long Should I Wait to Eat After Whitening?
Your best bet is to wait at least 30 to 60 minutes after a whitening session before eating or drinking anything besides plain water. Right after a treatment, your tooth enamel is temporarily more porous. This makes it a magnet for new stains and anything that might trigger sensitivity.
For the first 24 to 48 hours, sticking to a "white diet" is a really good idea. That just means picking foods and drinks that are light in color, not acidic, and served at a lukewarm temperature. Think plain chicken, rice, pasta, and lots of water. This protects your fresh results and keeps discomfort from creeping in.
Think of your teeth like a freshly painted wall right after whitening—they need time to set before being exposed to anything that could stain or damage the finish. A little patience goes a long way.
Does Sensitivity Toothpaste Weaken Whitening Results?
Nope, not at all. This is one of those myths that just won't go away, but there's no actual evidence that desensitizing toothpastes get in the way of the whitening process. Their active ingredients work by either calming the tooth's nerve or by blocking the tiny microscopic tubes in your dentin.
Neither of those actions stops the peroxide from getting into the enamel and breaking down stains. In fact, using a sensitivity toothpaste can actually help you get better whitening results. How? By making the whole thing more comfortable, it helps you stick to the full treatment schedule without having to quit early because of pain. It's truly a win-win.
At DentalHealth.com, we believe a brilliant smile should never come at the cost of comfort. Explore our curated selection of professional-grade desensitizing toothpastes, remineralizing pastes, and gentle whitening kits to build a routine that works for you. Find everything you need for a bright, pain-free smile at https://dentalhealth.com.

